How UT Research Led to the Development of the COVID-19 Vaccine in Record-Breaking Time
On January 6, 2020, Jason McLellan and his wife, Jinelle, were in Park City, Utah, for their family’s first-ever snowboarding vacation. It was a chance for the couple and their two young kids to relax after the holidays and before the spring semester kicked off at UT, when McLellan would begin his second year as an associate professor in molecular biosciences.
McLellan’s new snowboarding boots were pinching him, so he stopped at a shop to get them heat-molded to his feet. While he waited, McLellan saw Barney Graham’s name flash across his phone. The pair had first met in 2008 at the National Institutes of Health (NIH), where Graham is deputy director of the National Institute of Allergy and Infectious Diseases’ Vaccine Research Center, and McLellan was conducting his postdoctoral research in structure-based vaccine design after receiving his PhD from Johns Hopkins.
A mentor-mentee relationship quickly developed and now, more than a decade after meeting, the two scientists remain friends and frequent collaborators. Still, McLellan says, it was strange that Graham would pick up the phone and call him.
“Barney doesn’t call me often out of the blue, we normally email,” McLellan says. “I thought it was a Christmas thing.”
Graham wasn’t calling McLellan with belated holiday greetings, but to ask if he had heard about a new virus that had been discovered in China and was just beginning to get media coverage in the U.S.
“He told me that it looks like this new virus is actually a coronavirus, specifically a beta coronavirus, and similar to the original SARS coronavirus,” McLellan explains. “He said, ‘We don’t have the sequence yet, but as soon as we get it, are you ready to get back into the saddle and put teams together and quickly try and make a vaccine for it?’”
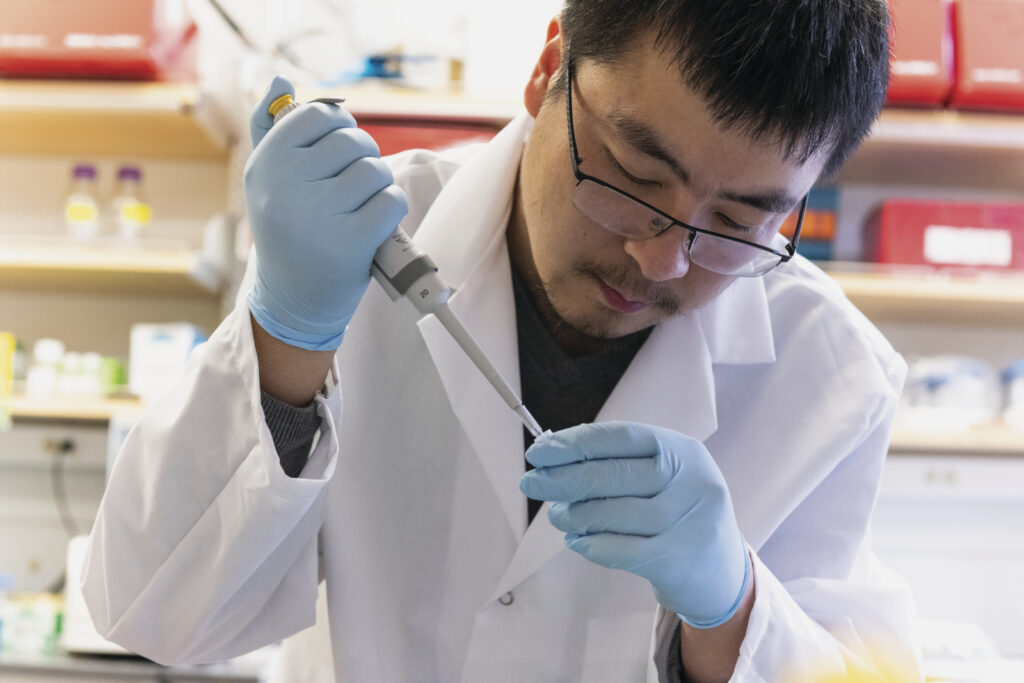
McLellan said he was, and opened WhatsApp to text Daniel Wrapp, one of his graduate students.
“Are you interested? Do you want to lead this?” he asked Wrapp.
“Yeah,” Wrapp replied, “let’s do it.”
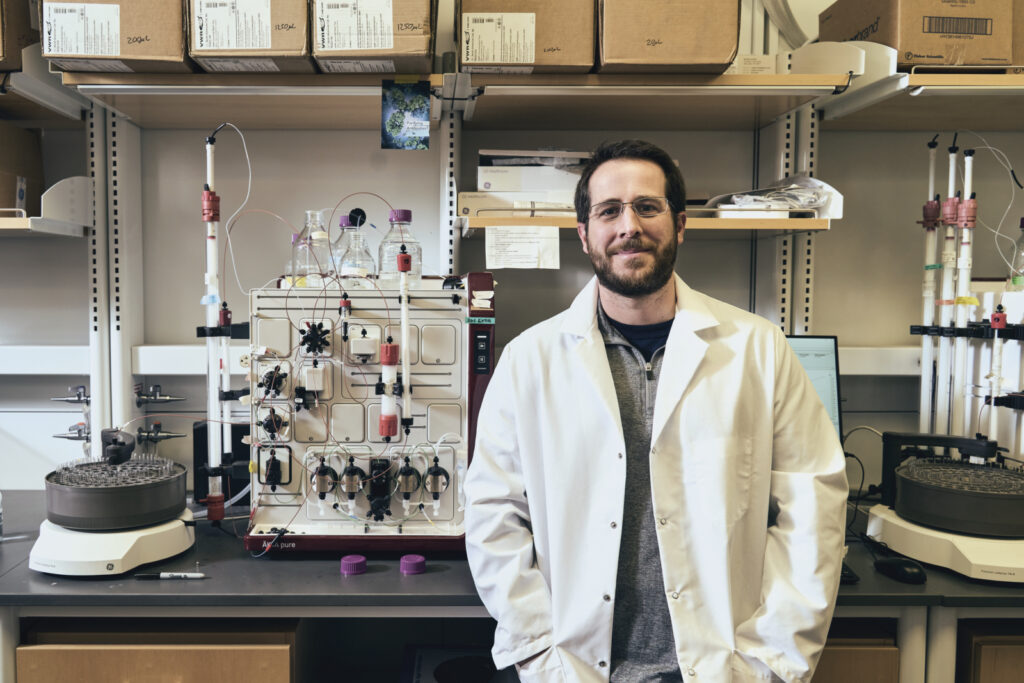
In 2018, McLellan came to UT from Dartmouth College, where he started the McLellan Lab five years earlier. In its relatively short history, the lab had developed a stellar reputation for its work in structure-based vaccine design, publishing papers in prestigious science journals, and attracting an all-star team of graduate and postdoctoral students. It also garnered the attention of Daniel Leahy, chair of Molecular Biosciences in the College of Natural Science, who also happened to be McLellan’s advisor at Johns Hopkins. With the resources of the UT System’s Science and Technology Acquisition and Retention (STARs) program, Leahy was able to lure McLellan and most of his team away from the Ivy League.
It was this team, led by McLellan, that would play a pivotal role in the creation of the COVID-19 vaccine, an inoculation to the virus that has killed hundreds of thousands of Americans and brought some of the world’s largest economies to a standstill. Using years of past research and collaborations with both the government and the pharmaceutical industry, the McLellan Lab was able to map the genetic code of the key spike protein, part of the virus that infects human beings and the crucial element in creating a “structure-based vaccine.” That spike protein would later be used in four early coronavirus vaccines, including the first two administered in the U.S. by Moderna and Pfizer. The path to mapping the spike protein that would save millions began with that unexpected phone call in Park City.
***
McLellan grew up outside of Detroit, near 8 Mile, a childhood he describes as lower-middle class. The first in his family to graduate from college, McLellan attended Wayne State University, where he enrolled as pre-med before switching his major to chemistry. “I wanted to help people,” he says. “I had [a] gift, I wanted to use it and … truly try and have an impact on human health.”
His journey from 8 Mile to the Forty Acres included stints at some of the most prestigious scientific institutions in the U.S.: Johns Hopkins University, the NIH, and the Geisel School of Medicine at Dartmouth College, which is where he was when he received an offer from The University of Texas to become an associate professor. Along with a promotion and tenure, the job also came with access to UT’s new multimillion-dollar Sauer Structural Biology Laboratory.
The Sauer Lab was funded by the Cancer Prevention Research Institute of Texas and Betsy Sauer, who asked for it be named in honor of her sister-in-law, Judy Camp Sauer, BA ’64. Housed in the Center for Biomedical Research Support, the institute boasts state-of-the-art technology, including the ability for cryogenic electron microscopy, or cryo-EM for short. Cryo-EM allows scientists to rapidly freeze atoms, thus capturing their shape when they are active. One scientist compared it to taking the face off a watch and looking at the gears.
“It was clear that to stay relevant in structural biology, you had to be able to do electron microscopy and have access to one of these state-of-the art facilities,” McLellan says, “and UT Austin had one that was brand new.”
And so, on a snowy day in January 2018, McLellan moved his family and nearly every member of his lab south to Austin. Wrapp was among the graduate students who had followed McLellan from Dartmouth to UT, a decision he says was an easy one.
“I applied to Dartmouth specifically because I hoped I would be able to join Jason’s lab,” Wrapp says. “So, when he told us he had made the decision to come to UT, it was a no-brainer for me to come along.”

Five days after messaging Wrapp from the mountain in Park City, McLellan was back on campus. In early January 2020, the world didn’t yet know it was on the brink of a pandemic. When Graham called him in Utah, McLellan thought this novel coronavirus could simply be an extension of the lab’s research on SARS and MERS, coronaviruses that emerged in 2002 and 2012, respectively.
“We didn’t know this was a once-in-a-century pandemic,” McLellan says. “In January and February there were still no [known] cases in the U.S., so it was hard to know if it was just a scientific exercise.”
On January 11, scientists in China had uploaded the first sequence of the novel coronavirus online, allowing researchers from across the globe free access to the virus’ genetic makeup. Within an hour, McLellan and his team had identified exactly what they wanted to isolate from the SARS-CoV-2 genome.
“We got the sequence, and it was similar to SARS coronavirus, and I immediately knew it was special and we had to pay attention,” says Nianshuang Wang, a postdoctoral fellow in McLellan’s lab from 2014 until this past August. “We knew SARS was very dangerous.”
Around the same time, Wang, following the news from his home country, started to get an inkling that this new virus might be more dangerous than its predecessors.
“I’m Chinese, so I was able to see and read what was happening [in China],” Wang says. “I [could] feel that something was happening.”
By February 19, McLellan’s team at UT and Graham’s team at the NIH had created the first 3D atomic scale map of the part of the virus that attaches to and infects human cells, a key breakthrough in the development of a COVID-19 vaccine.
“It blew everyone away how fast they got it done,” Leahy says. “In four weeks—four weeks!—they had determined a structure, written a paper, and had it accepted by Science. And this is work that historically would have taken multiple years. It’s a testament to the new cryo-electron microscopy methods as well as chance favoring the prepared mind.”
Meanwhile, at the NIH campus in Bethesda, Maryland, Graham was having conversations with Moderna, the biotechnology company that would later receive the first COVID-19 vaccine approval from the Food and Drug Administration. By March 16, just 63 days after Chinese researchers first posted the virus’ sequence online, Moderna released the first clinical batch of vaccines and the NIH announced the first person in the U.S. had been dosed.
Paul Goldbart, then-dean of the College of Natural Sciences—and McLellan’s boss—characterizes this partnership between UT, the NIH, and Moderna as a “triumvirate of industry.”
“University, government, and industry—they are like three legs of a stool,” he says, “and you need all three in a crisis.”
By mid-March, COVID-19 had hit Texas, and though they didn’t know it at the time, UT students leaving for spring break would not be returning to campus. At the lab, McLellan maintained a steady pace, working six days a week and foregoing his family’s two-week trip back home to Michigan.
With vaccine trials underway, McLellan and his team turned their attention to a llama named Winter. In 2016, the researchers were studying SARS-CoV-1 and MERS-CoV-1. Currently, there are seven known coronaviruses in the world, four of which cause the common cold. SARS and MERS, however, had proved far more lethal than the others. Though their mortality rates are high—11 percent for SARS-CoV-1 and 35.2 percent for MERS-CoV-1, according to the NIH—they are much harder to transmit than SARS-COV-2, the virus that causes COVID-19. Before it disappeared in 2004, SARS caused 916 deaths across the globe while MERS, which is still in existence but hasn’t spread much beyond the Middle East, has killed 811 people worldwide.
“In 2013, we were like let’s try to do structure-based vaccine design for a coronavirus; let’s try and make a MERS vaccine,” McLellan says. “We had a coronavirus emerge in 2002 [and] 2012, there’s probably another one in 2022. So, let’s start figuring out how to make coronavirus vaccines.”
Though the next coronavirus came a few years earlier than they predicted, the researchers found a key element to combat COVID-19 in an experiment conducted in 2016. Along with the NIH and Ghent University in Belgium, UT researchers had injected the then-9-month-old llama with stabilized spike proteins from those two viruses.
Winter, like all llamas, produces two types of antibodies: one similar to human antibodies and one about a quarter of the size, which is sometimes referred to by researchers as a nanobody. Antibodies are important because, unlike a vaccine, they can be given to patients directly to help combat the disease. Nanobodies are important because they can be nebulized and inhaled right to the site of the infection. (For the record, Winter still lives on a farm in Belgium, unaware of her contribution.)
“That was exciting to me because I’d been working on this for years,” Wrapp said in an April 29, 2020, press release. “But there wasn’t a big need for a coronavirus treatment then. This was just basic research. Now, this can potentially have some translational implications, too.”
Far beyond “translational implications,” the discoveries made with Winter have gone on to save countless lives. And they illustrate the importance of investing in science, from the halls of government to the labs of research universities like UT—and even the fields of Belgium.
“I think it validates our belief that science is important and long-term investment in basic science really is just that: an incredible investment,” Leahy says. “In this particular case, it allowed us, meaning the scientific community, to develop this vaccine in absolutely record time. Had this investment not been made 10 years ago, we’d still be in the early stages.”
With the vaccine rollout underway, the researchers are taking a well-deserved victory lap in the media. Since December, they have been featured, among other places, in the Washington Post, National Geographic, This American Life, and a 30,000-word New Yorker article by Pulitzer Prize-winner Lawrence Wright. In December, McLellan and his team were among those awarded the Golden Goose, an award that highlights “seemingly obscure studies that have led to major breakthroughs and resulted in significant societal impact.”
When asked if he knew on January 11, 2020, that what he was working on would change the world, McLellan says, “Nope.”
“Do you know now?” I ask.
The professor smiles. “Yup.”
[WATCH: UT Austin Associate Professor Jason McLellan on Working Toward a Coronavirus Vaccine]














No comments
Be the first one to leave a comment.