By Aran Sullivan
THE IDEA
Many melanoma patients are treated with drugs called BRAF or MEK inhibitors that specifically target the mutant proteins created in cancerous tumors. These inhibitors can block the tumors’ ability to grow and spread.
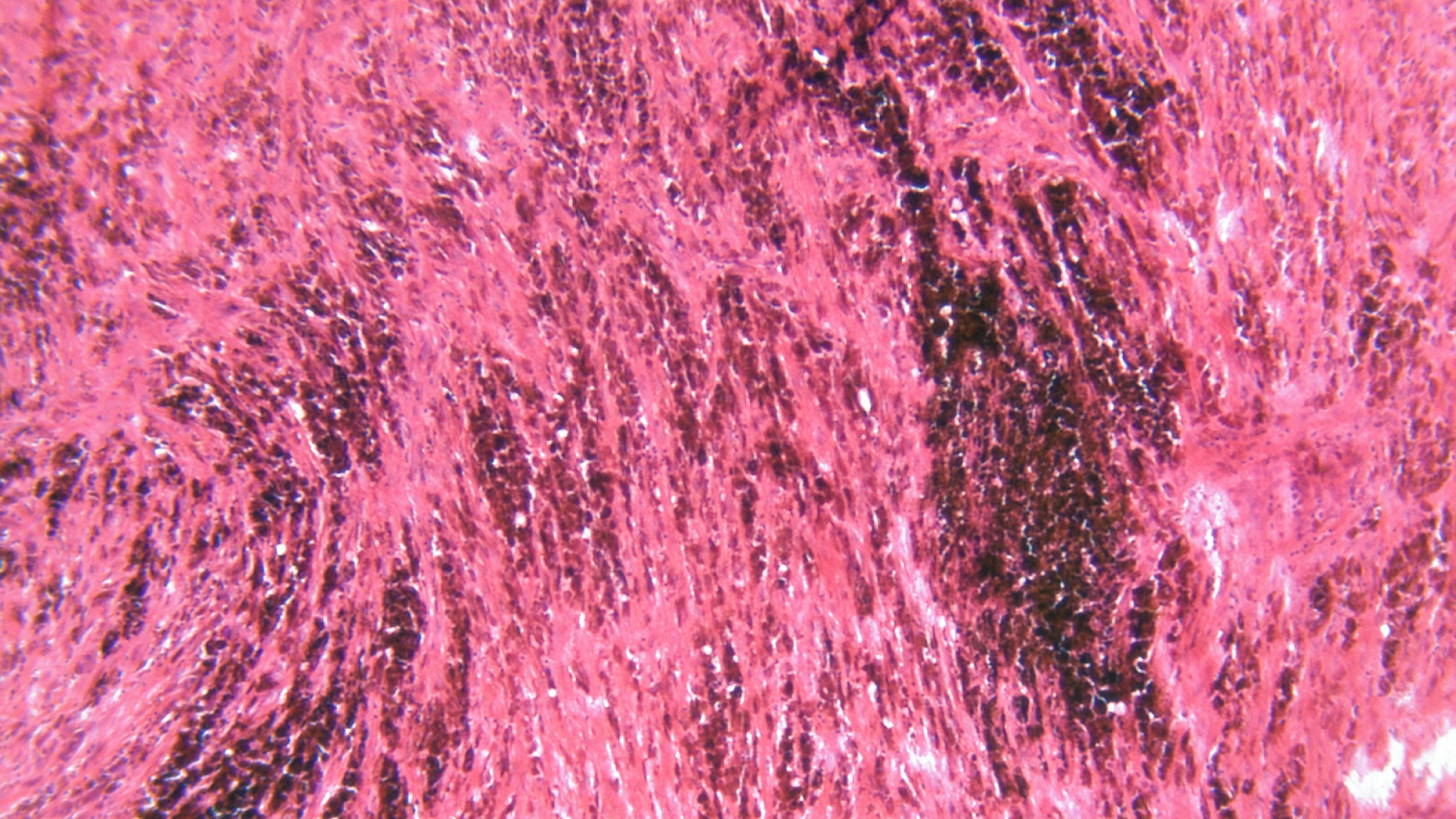
According to Ann Richmond, Ingram Professor of Cancer Research and professor of pharmacology and dermatology, while these inhibitors are shown to be rapidly effective and to increase survival rates, most patients eventually experience relapse. To help solve this problem, Richmond and other researchers at Vanderbilt School of Medicine Basic Sciences used spatial imaging analysis of tissues. These imaging techniques allowed researchers to investigate the properties of the tumors and immune cells in patients before and after developing resistance to the BRAF and MEK inhibitors.

When observing post-treatment resistant tumors, Chi Yan, research assistant professor of pharmacology and first author of the study, found significantly more melanoma cells with biomarker SOX10 present, indicating that these cells may be treatment-resistant. SOX10 plays a role in the differentiation of precancerous cells into cancerous melanocytes, which are skin cells associated with skin pigmentation. Presence of SOX10 is thought to create an environment that blocks the immune system from being able to regulate tumor growth, and loss of expression of SOX10 is associated with reduced tumor formation.
WHY IT MATTERS
Melanoma is the fifth most-common type of cancer in the U.S., and, according to the American Cancer Society, about half of patients with malignant melanoma have mutations of the BRAF gene. Identification of potential tumor biomarkers such as SOX10 can help physicians better predict outcomes for their patients.

“Our findings may indicate that those melanoma tumor cells that develop resistance to BRAF/MEK-targeted therapy express more SOX10, which suppresses the anti-tumor immune response,” Yan said. While it is too early to declare SOX10 expression by melanoma cells as a marker for resistance to BRAF/MEK inhibitors, the findings have promise in helping oncologists improve their knowledge and understanding of why resistance to therapy occurs.
“Our study highlights the fact that cancer progression can occur despite the proximity of immune cells to cancer cells. This suggests that therapy-resistant tumor cells are associated with an environment that can inactivate those immune cells, and this leads to overall acquired treatment resistance,” Yan said.
WHAT’S NEXT
“Further studies are needed to understand the crosstalk between rapidly dividing SOX10+ melanoma cells and the close-by immune cells,” Yan said. “The mechanism by which the tumor cells influence the immune cells is still an important question, and these interactions are likely contributing to acquired resistance in BRAF/MEK-targeted therapies.”
FUNDING
This research was supported by a VA Merit Award, an SRCS award to Ann Richmond, R01 grant support from the National Cancer Institute and the NCI Vanderbilt Ingram Cancer Center Support Grant.
GO DEEPER
The study, “Proximity of immune and tumor cells underlies response to BRAF/MEK-targeted therapies in metastatic melanoma patients,” was published in the journal npj Precision Oncology on Jan. 20.
“This work was a team effort that was greatly facilitated by co-authors Sheau-Chiann Chen, Dan Ayers, Caroline Nebhan, Joseph Roland, Vivian Weiss and Doug Johnson,” said Richmond, who is also a research career scientist with the Nashville VA Medical Center.